A fascinating new study, published in the Journal of Clinical Investigation, has revealed an unexpected potential benefit of severe COVID infection: it may help shrink cancer.
This surprising finding, based on research conducted in mice, opens up new possibilities for cancer treatment and sheds light on the complex interactions between the immune system and cancer cells – but it certainly doesn’t mean people should actively try to catch COVID.
The data outlining the importance of the immune system in cancer is considerable and many drugs target the immune system, unlocking its potential, an important focus of my own research.
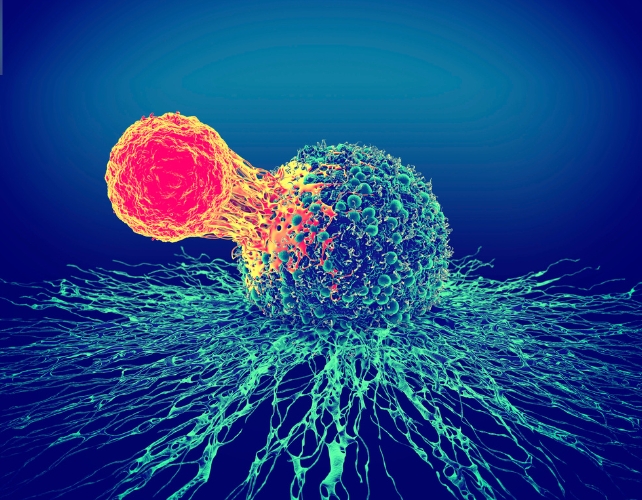
The study here focused on a type of white blood cell called monocytes. These immune cells play a crucial role in the body’s defence against infections and other threats.
However, in cancer patients, monocytes can sometimes be hijacked by tumour cells and transformed into cancer-friendly cells that protect the tumour from the immune system.
What the researchers discovered was that severe COVID infection causes the body to produce a special type of monocyte with unique anti-cancer properties. These “induced” monocytes are specifically trained to target the virus, but they also retain the ability to fight cancer cells.
To understand how this works, we need to look at the genetic material of the virus that causes COVID. The researchers found that these induced monocytes have a special receptor that binds well to a specific sequence of COVID RNA.
Ankit Bharat, one of the scientists involved in this work from Northwestern University in Chicago explained this relationship using a lock-and-key analogy: “If the monocyte was a lock, and the COVID RNA was a key, then COVID RNA is the perfect fit.”
Remarkable
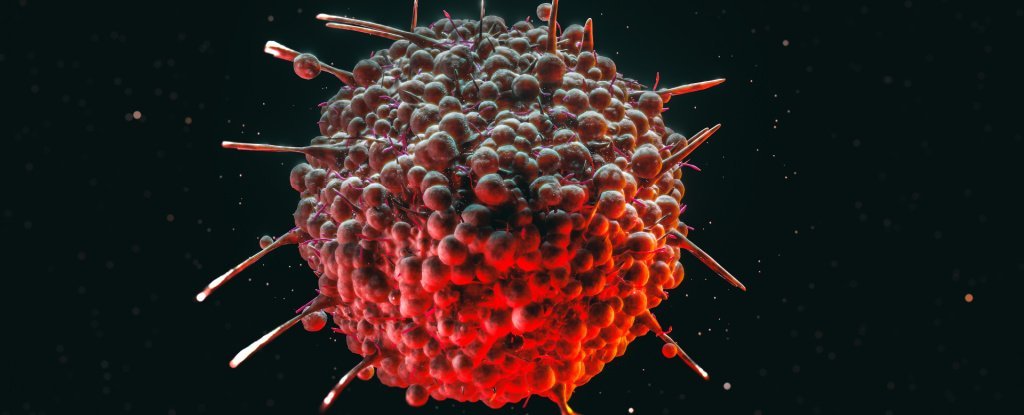
To test their theory, the research team conducted experiments on mice with various types of advanced (stage 4) cancers, including melanoma, lung, breast and colon cancer.
They gave the mice a drug that mimicked the immune response to a severe COVID infection, inducing the production of these special monocytes. The results were remarkable. The tumours in the mice began to shrink across all four types of cancer studied.
Unlike regular monocytes, which can be converted by tumours into protective cells, these induced monocytes retained their cancer-fighting properties. They were able to migrate to the tumour sites – a feat that most immune cells cannot accomplish – and, once there, they activated natural killer cells.
These killer cells then attacked the cancer cells, causing the tumours to shrink.
This mechanism is particularly exciting because it offers a new approach to fighting cancer that doesn’t rely on T cells, which are the focus of many current immunotherapy treatments.
While immunotherapy has shown promise, it only works in about 20% to 40% of cases, often failing when the body can’t produce enough functioning T cells. Indeed it’s thought that the reliance on T cell immunity is a major limitation of current immunotherapy approaches.
This new mechanism, by contrast, offers a way to selectively kill tumours that is independent of T cells, potentially providing a solution for patients who don’t respond to traditional immunotherapy.
It’s important to note that this study was conducted in mice, and clinical trials will be necessary to determine if the same effect occurs in humans.
Maybe aspects of this mechanism could work in humans and against other types of cancer as well, as it disrupts a common pathway that most cancers use to spread throughout the body.
While COVID vaccines are unlikely to trigger this mechanism (as they don’t use the full RNA sequence as the virus), this research opens up possibilities for developing new drugs and vaccines that could stimulate the production of these cancer-fighting monocytes.
Trained immunity
The implications of this study extend beyond COVID and cancer. It shows how our immune system can be trained by one type of threat to become more effective against another.
This concept, known as “trained immunity”, is an exciting area of research that could lead to new approaches for treating a wide range of diseases.
However, it’s crucial again to emphasise that this doesn’t mean people should seek out COVID infection as a way to fight cancer, and this is especially dangerous as I have described. Severe COVID can be life-threatening and has many serious long-term health consequences.
Instead, this research provides valuable insights that could lead to the development of safer, more targeted treatments in the future. As we continue to grapple with the aftermath of the COVID pandemic, new infections and long COVID, studies like this remind us of the importance of basic scientific research.
Even in the face of a global health crisis, researchers are finding ways to advance our understanding of human biology and disease. This work not only helps us combat the immediate threat of COVID, but also paves the way for breakthroughs in treating other serious conditions such as cancer.
While there’s still much work to be done before these findings can be translated into treatments for human patients, this study represents an exciting step forward in our understanding of the complex relationship between viruses, the immune system and cancer.
It offers hope for new therapeutic approaches and underscores the often unexpected ways in which scientific discoveries can lead to medical breakthroughs.![]()
Justin Stebbing, Professor of Biomedical Sciences, Anglia Ruskin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.









Leave a Reply